.gif)
.gif)

|
Imaging in Developing Countries |
|
Special Interest Group |









|
I completed my PgD in Medical Ultrasound last year and towards the end of my training decided it might be useful to do a month long elective in a developing country to observe the use of radiography and specifically ultrasound in this setting. |
|
|
|
I contacted a small hospital in rural Uganda that I had heard about through some friends who had visited for their medical electives. They said that they would be delighted to have an ultrasound ‘expert’ visit as they had recently acquired an ATL 5,000 machine but did not have a member of staff qualified to operate it. This was obviously unnerving but I decided that I should give it go. |
|
|
|
|
|
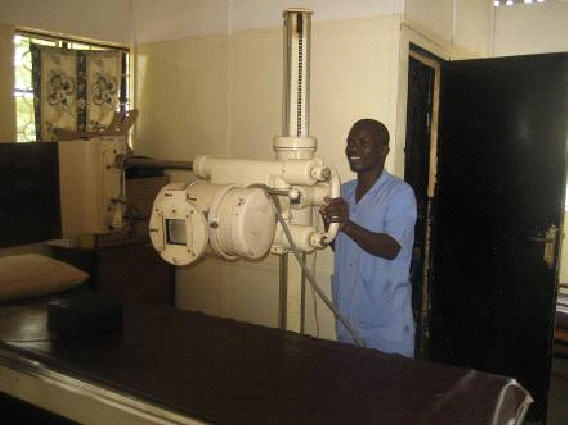
The Hospital is a non-profit charity hospital and has only 5 doctors for 222 beds. Approximately 32,000 outpatients and 7,000 inpatients are served by the hospital each year |
.gif)

|
Report on Visit to Kiwoko Hospital, Uganda |
|
Many of the patients I scanned were in end-stage phases of their illnesses and were often full of free fluid and non-functioning organs- death was a regular occurrence. |
|
I saw several cases of end stage hepatitis B with chronic liver failure as well as a number of end stage renal-failure cases and some severe cholangitis. Many patients had advanced AIDS and associated pathology. I certainly felt quite out of my depth in my first week, but since they had no qualified sonographer, the doctors were relying on my opinions quite a bit. |
|
Although English is the official language of the country, most patients spoke only their native language therefore communication was often extremely difficult. |
|
One patient came into the hospital complaining of an abdominal mass and when I scanned her I discovered an 18 week live foetus. She did not understand this and claimed that she was a virgin and it was not possible. When I fetched one of the Ugandan doctors to explain in her native tongue she still wouldn't accept. The doctor explained to me that it is a sad fact that many young girls are sexually abused by family members and often don't understand what is happening to them. |
|
The suffering caused by the Ugandan civil war is also still evident today. One patient I met was blind after having his eyes removed as a form of torture and was left caring for his two small grandchildren after the death of their parents. |
|
|
|
Only one doctor and one midwife at the hospital had some basic ultrasound knowledge and much of my time was occupied with teaching them how to get the best out of the equipment and how to make accurate measurements. As a newly qualified sonographer, teaching was a completely new area for me however I saw significant improvements in ultrasound practice particularly by the midwife in a relatively short time. |